Letter From the CEO: Why CancerIQ is Furthering Our Investment in Tools for Genetic Counselors
Genetic counselors are an invaluable resource for early cancer detection and precision cancer prevention. Today this limited workforce is focused on...
We speak with clients all of the time who are facing challenges justifying the investment in personnel and software support required to start, run, or grow their cancer genetic counseling and high risk programs.
In this post, we’ll teach you how to forecast the ROI of your cancer genetics or high risk program so you can get resources for the people, tools, and processes needed for success. We'll discuss:
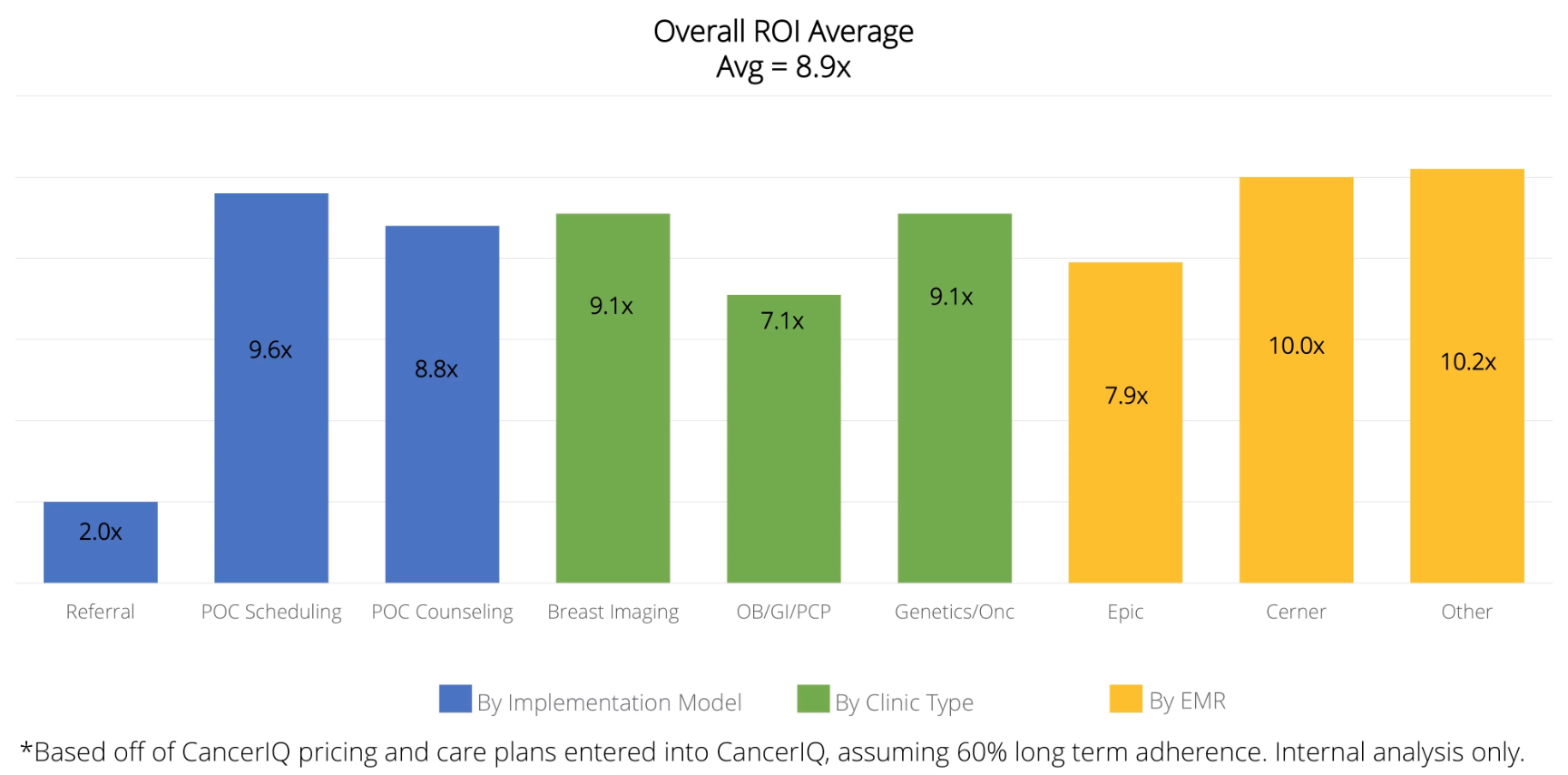
The team at CancerIQ is extremely data-driven, and has benchmarked both clinical, operational, and financial outcome data across the dozens of hospital systems that work with us. To understand the source of the case studies and figures presented in our analysis, here is the data set we are working with:
Our track record comes from implementing CancerIQ in a diverse range of clinical environments. Our clients have chosen different implementation models, deployed CancerIQ in a broad range of clinical settings, and have operated CancerIQ alongside a diverse range of existing HIT systems.
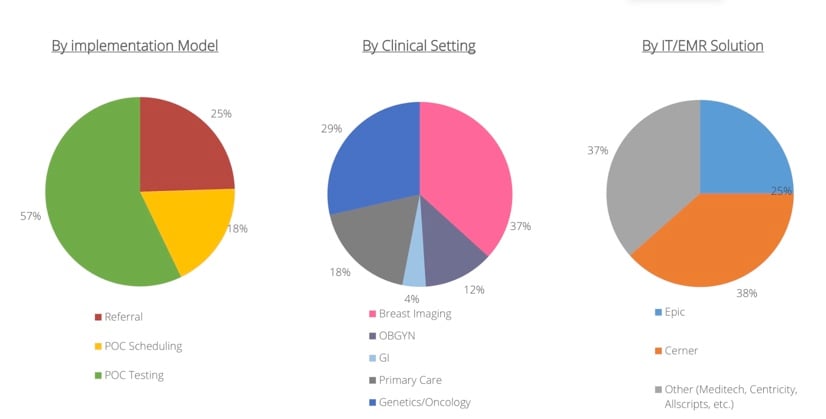
Despite the diverse clinical settings we operate in, the fundamental drivers of ROI are the same. And when applied across our health system clients - we have seen consistently high ROI across nearly all of our client categories.
First off, when determining the ROI, it’s important to look at these three categories:
We’ll take a look at each one of these areas and provide a few examples from our clients showing how they turned their program into a source of revenue for the health system (with a little help from CancerIQ).
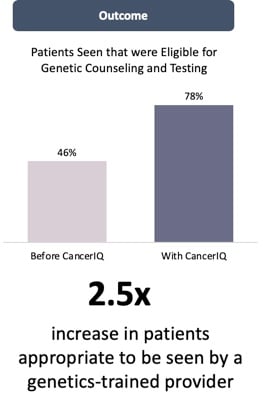
Identifying patients eligible for genetic evaluation services is at the top of the funnel, and the first lever to pull to generate an ROI on your high risk program
One of our clients, Marin General Hospital, started their program using the Tyrer-Cuzick score embedded in their radiology information system.

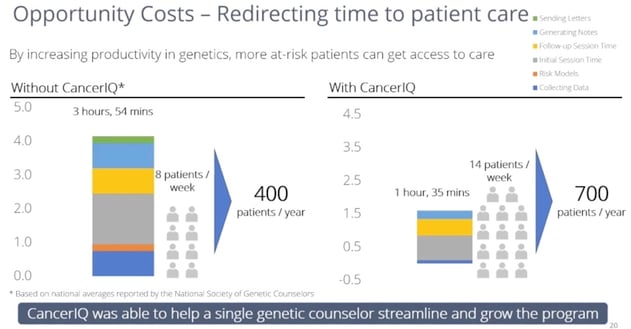
According to the National Society of Genetic Counselors, an average genetic counselor sees 10 patients per week. Unlike other medical professionals, they have triple the documentation burden (generating notes for patients, providers, and insurance companies), and they spend a lot of time gather data using interview-based techniques. Based on time studies observed in dozens of practices across the country - these non-clinical tasks are the primary cause for constraints in genetic counselor capacity.
Read insights from Maritess Caamic, Director of the Cancer Institute and Infusion Services at Advocate Illinois Masonic Medical Center in our previous post "10 Cancer Risk Assessment Questions Every Administrator Has"
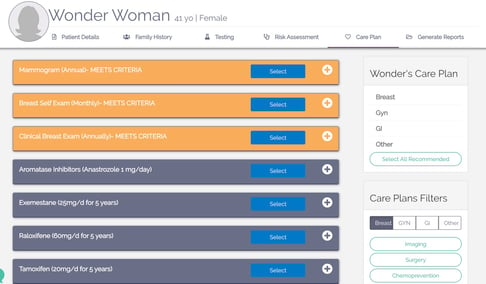
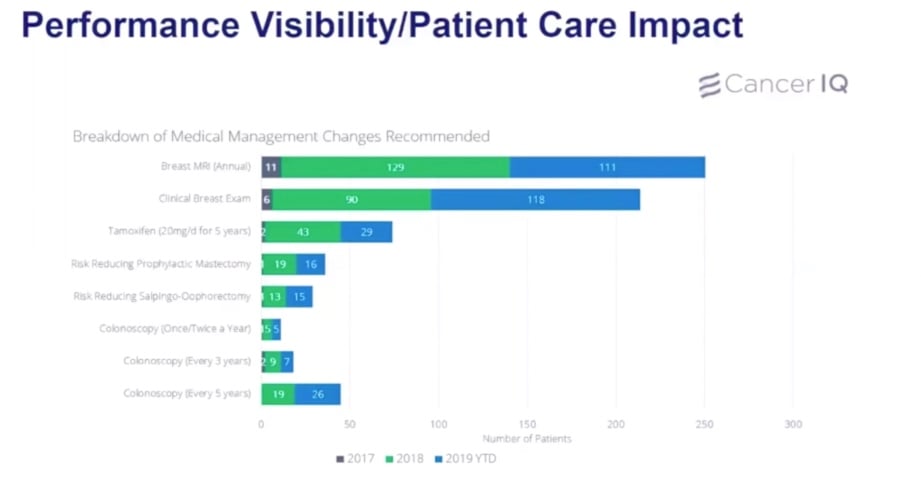
The greater opportunity with a cancer genetics program is not the direct revenue, but the downstream revenue that comes from the management of patients classified at increased risk. Genetic counselors will recommend a change in medical management for 40% of patients they see, with 10% of patients testing positive, and approximately 30% of patients testing negative for remaining at elevated risk due to familial risk factors. To demonstrate the potential downstream revenue potential, we'll share a case study from a breast center, and from a cancer center's perspective.
The specific revenue opportunities in a breast center staffed by a high risk nurse practitioner include:
The following case study is how one high risk breast program was able to deliver on their promise of downstream revenue
Hear more from Michele Settelmyer, Risk Assessment APN at OSF Healthcare, in our webinar: Implement a Genetic Screening and Navigation Program in an Imaging Center
A genetic counseling program within a cancer center has a different set of downstream revenue opportunities than a breast center based program, as they typically serve a broader range of affected and unaffected patients, and make recommendations for management of non-hereditary breast and ovarian cancer conditions. The following case study shares the experience of Sharp Healthcare, whose results were published in the Advisory Board:
As seen in the Marin Case Study, the return on investment in a comprehensive high risk program can depend heavily on the volume of patients at the top of the funnel.
If you have a genetic counselor and are trying to estimate the productivity gains for your organization, assume that the current staff you have offering genetic counseling services will be able to see up to 2x the number of patients within the first year using CancerIQ.
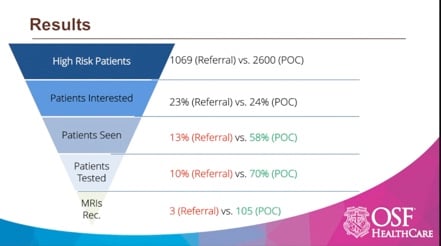
If you don't have a genetic counselor and are trying to estimate the percentage of patients identified that will be seen by a newly formed genetic counseling position, assume that patient uptake will be dependent on the implementation model that you choose. According to our data, patient uptake is:
On average, assume that 10% of patients seen by your high risk specialist will test positive, and 30% will test negative.
For the patients who test positive, assume they will choose the following risk reduction strategies:
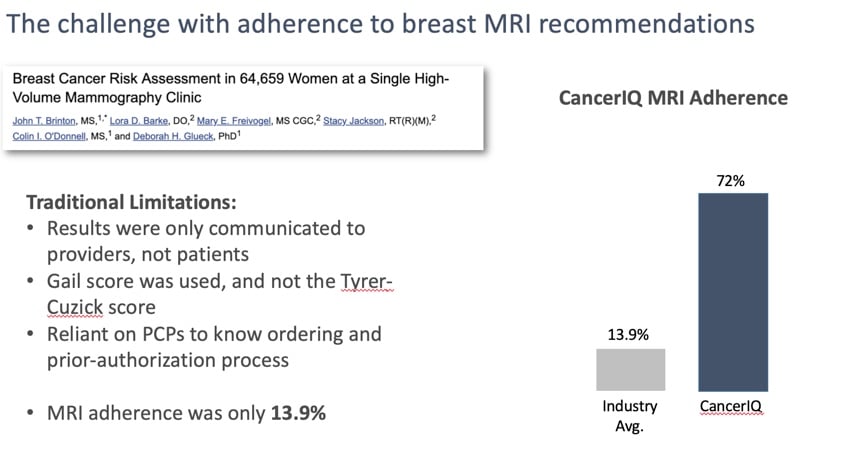
As we've learned from several implementation models, patient compliance with medical management recommendations can vary based on the workflow of your high risk program. If there is not a formal infrastructure in place to follow up with patients and their providers, we have found adherence numbers to be incredibly low. To inform this assumption, we have looked closely at adherence rates pre and post implementation of CancerIQ.
No formal process in place - 80% of patients that test positive will comply, but only 25% of high negatives may comply with their medical management plan.
Software-enable process: 85%-90% of patients that test positive will comply, and 60% of high risk negatives will comply. Through ongoing patient reminders and visual queues for the provider to act on
While certain procedures are one-time events, the majority of patients with a high risk diagnosis are going to be on a high risk surveillance plan for the rest of their lives. This means that your ROI will not only be driven by revenues generated on a one-time basis, but for years to come.
If your institution is preparing to shift from fee-for-service to fee-for-value, it is critical to think through these financial matters so you're prepared for the change in business model.
Because what does this mean in practice? It's time to act now and invest in stratifying your patient population as soon as possible. You will want to complete all the costly risk reducing procedures before value based contracts kick in. You will want to know how many high risk patients will need high risk surveillance services before negotiating bundled payments for your population.
Here's the good thing - developing a hereditary cancer risk assessment program is a win-win in all healthcare business model. Mutation carriers are typically at risk for extremely costly, early onset cancers - and implementing a hereditary cancer screening program to avoid those cancers will help prevent those outlier cases down the line.
If your head is spinning after this article and you need some help calculating an ROI and making the case for your program, we're here to help.
Click below to access a member of our team and our ROI calculator.
References[1] Rosenthal et al. Outcomes for Clinical Testing on 76,000 Patients Using a Panel of 25 Genes Associated with Risk of Breast, Ovarian, Colorectal, Endometrial, Gastric, Pancreatic, Melanoma, and Prostate Cancers. Abstract 1515 Presented at ASCO, June 2015
[2] Plevritis SK, Kurian AW, Sigal BM, et al. Cost-‐effectiveness of screening BRCA1/2 mutation carriers with breast magnetic resonance imaging. JAMA : the journal of the American Medical Association. May 24 2006;295(20):2374-‐2384.
[3] Warner E, Plewes D, Causer P, et al. Effect o Age and Temporal Patterns Over 5 years in a magnetic resonance imaging (MRI)-‐based Breast Surveillance Study for BRCA Mutation Carriers. ASCO Annual Meeting; 2004; New Orleans.
[4] Consumer price index-‐medical care, all urban consumers (US city average, not seasonally adjusted) http://data.bls.gov/cgi-‐bin/print.pl/news.release/cpi.nr0.htm. Accessed Dec 5th, 2016.
[5] Grann VR, Patel PR, Jacobson JS, et al. Comparative effectiveness of screening and prevention strategies among BRCA1/2-‐affected mutation carriers. Breast cancer research and treatment. Feb 2011;125(3):837-‐847.
[6] Red Book Pharmacy's Fundemental Reference. Montvale, NJ: Thomson PDR; 2008.
Genetic counselors are an invaluable resource for early cancer detection and precision cancer prevention. Today this limited workforce is focused on...
Feyi Olopade was named to Crain's 40 under 40 list. While she is doing great things at CancerIQ, her rescue dog, Ricky, stole the spotlight.
OSF HealthCare, one of our longstanding partners, recently enhanced their program with a hybrid HL7 and FHIR integration with CancerIQ to integrate...
CancerIQ is proud to offer precision prevention news and learning opportunities to our clinical champion community. You don't have to be our customer to take advantage – subscribe to receive the content you care about.