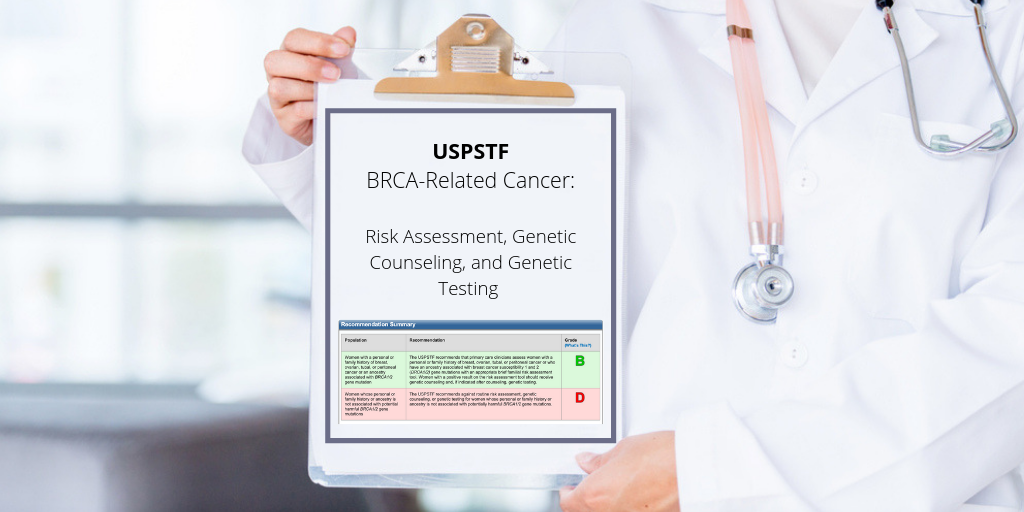
Primary care clinicians should assess women with a personal or family history of breast, ovarian, tubal, or peritoneal cancer or who have an ancestry associated with BRCA1 and BRCA2 gene mutations, according to new recommendations from the US Preventive Services Task Force (USPSTF).
The latest recommendations expand who should receive risk assessment for harmful BRCA1/2 genes to include women who personally have been diagnosed with hereditary breast and ovarian cancer, and individuals of ancestries like Ashkenazi Jewish descent who are more likely to develop breast cancers.
What may be receiving less attention, though, is the recommendation that primary care physicians use validated risk assessment tools before referring patients for genetic counseling and testing. So what does this mean? And how should primary care providers implement a familial risk assessment tool into routine cancer screening?
Here are three key insights from the USPTF guidelines to answer those very questions.
Insight #1: We're Not in a Population Genetic Testing Era Yet
Because inherited BRCA1 and BRCA2 mutations account for up to 10 percent of breast cancer cases, the USPSTF explicitly recommended against population genetic testing for BRCA genes. There is little evidence that ordering genetic testing for patients that don’t meet criteria has a clinical benefit. The “test everybody” concept could cause more harm than good.
Insight #2: Risk Assessment is a More Appropriate Next Step for Primary Care Providers
To identify high-risk patient populations, the USPSTF recommended that primary care physicians use validated screening tools that flag patients who meet the updated criteria.
In a JAMA editorial regarding the updated guidelines, authors from the University of Chicago wrote, "Forms of the USPSTF guidelines have been in place for more than a decade, but PCPs need adequate tools to participate fully in preventive oncology." As we learned from this Health Data Management report, printing out of the validated tools can be disruptive to workflow and stressful for staff.
Insight #3: Ordering a Test and Completing a Risk Assessment Require Different Levels of Effort
In the population screening scenario, ordering a genetic test without conducting a familial risk assessment could be relatively easy to do in a primary care setting. In this futuristic world - where, for example, ordering a genetic test is as easy as ordering a complete blood count (CBC) - fitting this into the routine annual visit workup (assuming no genetic counseling) is clinically and operationally feasible.
But completing a family history-based risk assessment, and referring patients to genetic counseling is a far different task. The need to gather a non-clinical history and keep track of increasingly blended ethnicities could make it more difficult.
This more cumbersome process could allow for more BRCA carriers to fall through the cracks, as it already is today. According to Childers et al, fewer than one in five individuals who meet criteria have been tested, suggesting that this "family history screen + genetic counseling referral" process isn't working.
Three Challenges to Implementing Risk Assessment in Routine Care:
(1) Garbage In, Garbage Out
The quality of a risk assessment is only as strong as the quality of the data collected about the patient’s personal and family cancer history.
Why? Providers lack the time. From what we’ve learned implementing software in primary care settings and integrating with various electronic medical records (EMRs) – there is very little time for providers to gather a complete family history on every patient. And when they do, turning their back to the patient to live-enter this data into a clunky EMR never happens. According to study results presented at the 2019 American Society of Clinical Oncology (ASCO) Annual Meeting, less than half (46.7 percent) of patients with breast cancer provided sufficient family history necessary for predicting risk. The consequences? Poor data. Inaccurate risk assessments. Lower quality clinical care.
(2) Lack of Actionability
In clinical settings without genetic counselors, there can be a lack of actionable next steps.
Without a pathway for patients to access genetic counseling and testing, primary care providers now have knowledge about risk factors they feel medically liable for. This is akin to identifying a patient with heart disease, and having no way to refer to a cardiologist to manage that disease over time. The referral pathway to genetic counseling is even worse – the American College of Cardiology reports that there are over 23,000 cardiologists vs. the 697 cancer-specific genetic counselors that the National Society of Genetic Counselors reported in their 2019 Professional Status Survey.
The referral pathway through genetic counseling can also create unintended disparities in testing rates across ethnic groups. According to a 2017 study by Whitworth et al, of those patients referred to genetic counseling, cancellation rates were highest amongst minority groups compared to individuals of European ancestry:
- 48.9 percent of African American patients cancelled
- 49.6 percent of Latino patients cancelled
- 33.9 percent of Caucasian patients cancelled
If primary care providers don’t see a path for their patients to act on, or assume their patients won't go through with it, then why do a risk assessment at all? This is why innovative solutions like clinically integrated telehealth genetic counseling are important; it can help provide a more direct path for patients to access genetic counselors remotely. Based on what we've learned from this Health Data Management article, or this Oncology Nursing News article, patient compliance improves when telehealth services are accessible on site, or scheduled immediately at the point of care.
(3) EMR Integration
Primary care providers live in the EMR, so this tool needs to be already integrated with the technology you already have.
Primary care providers live in the EMR, so incorporating risk assessment into EMR systems will increase the likelihood of success. While this seems like a relatively easy feat - the evidence-based criteria for determining eligibility for genetic counseling and testing moves at too rapid a pace for traditional EMR vendors to keep up.
This is exactly why solutions like CancerIQ exist, and why forward-thinking health systems with established cancer risk assessment and prevention programs have integrated these solutions into the EMR.
Making Risk Assessment Part of Routine Medical Care
Though expanding risk assessment to a broader set of women presents a challenge, it is a challenge worth tackling. There are aspects of patient care that are difficult for primary care providers to control - such as obesity, which studies show are difficult for primary care providers to manage without psychosocial / behavioral support. But an early diagnosis of cancer is well within a primary care provider's control. Telling a BRCA mutation carrier to come in early for mammograms and MRIs, or referring a BRCA-related breast cancer survivor to consider removing her ovaries are all life-changing interventions within their purview.
We are excited about these new recommendations, and the continued validation of the need for genetic information to be used in preventive care. Mary-Claire King summarizes this sentiment well in a 2014 JAMA article: "To identify a woman as a carrier only after she develops cancer is a failure of cancer prevention."
So, how can primary care leverage technology to meet these new recommendations?
In part two of the series, we explore this very question. Specifically, we show how primary care providers are solving some of the challenges discussed above, like:
- Streamlining the data collection process,
- Leveraging telehealth genetic counseling, and
- Getting this all into their EMRs.
