The stats are well-known by now. The U.S. spends nearly 18 percent of its GDP on healthcare, which is about twice that of other high-income nations. However, despite the amount of money poured into providing care, the U.S. tends to rank lower in the world with respect to the quality of that care.
The main message from these figures has consistently been that the health of people and populations depends on the consistent performance of the health systems providing that care. Hence, the healthcare industry’s shift from fee-for-service to value-based care.
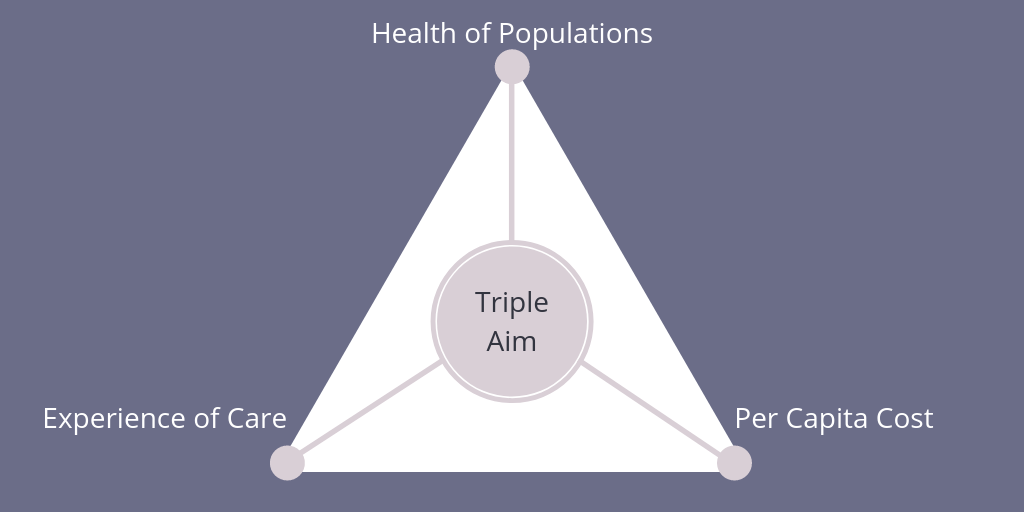
Much has been made about how to make this shift—and when it will be completed—but there seems to be universal alignment on the final destination. And one commonly accepted framework for achieving the vision of value-based care is the Triple Aim.
What is the Triple Aim?
Introduced by the Institute for Healthcare Improvement (IHI), the Triple Aim focuses on the simultaneous pursuit of three dimensions:
- Improving the individual experience of care.
- Improving the health of populations.
- Reducing the per capita costs of care for populations.
Though current approaches to the triple aim have primarily focused on managing chronic conditions, cancer risk assessment and genetics are one area in which health systems can become more proactive and achieve a stronger patient experience of care, improve the health of their populations, and reduce the cost of that care.
Why Cancer Risk Assessment and Genetics?
Advances in genome sequencing have enabled widespread adoption of affordable genetic testing that can identify patients at increased or high risk for hereditary cancer - which accounts for up to 10 percent of new diagnoses, according to the National Cancer Institute. These cancers tend to be earlier onset, and more aggressive, so genetic testing is key to decreasing treatment costs and improving survival.
Cancer risk assessment and genetics can help drive the Triple Aim framework within health systems in the following three ways:
- Improving the patient experience of care. Genetic evaluation empowers providers with better data, which can be used to deliver more safe, effective, patient-centered, timely, efficient, and equitable care.
- Improving the health of populations. Providers can flag all patients according to their level of risk for hereditary cancers, give at-risk patients access to genetic counseling, and manage those patients according to their genetic risk factors using the latest National Comprehensive Cancer Network (NCCN) Guidelines.
- Reducing the per capita cost of care. A late-stage cancer diagnosis is incredibly costly. Cancer risk assessment can help lead to an earlier stage diagnosis for cancers that are easier to treat.
Why is This Not Happening Today?
With only about 4,000 practicing genetic counselors nationwide - which is one for every 80,000 Americans - the traditional model of referring out for testing is not scalable nor reliable. This can negatively impact both the patient experience of care and outcomes.
To ensure populations receive standardized care, health systems need to meet patients where they are and create a seamless continuum of care no matter the practice type or geographic setting. But the current patient experience is disjointed.
Likewise, cancer risk assessment and genetics is most commonly limited to specialty services. But by integrating beyond specialty services into routine care settings like OB/GYN and primary care, health systems can begin to stratify patient populations based on genetic risk factors for a true population health strategy.
Quantifying the impact cancer risk assessment and genetics have on reducing the per capita cost of care can be difficult. Most health systems may only focus on the value of an initial genetic counseling appointment. To realize the true impact, however, health systems should look beyond the initial consultation at the potential downstream revenue from increased surveillance and preventive services.
Innovative Solutions That Are Making Risk Assessment and Genetics More Accessible
To overcome these common challenges, several health systems have adopted innovative approaches to delivering cancer risk assessment and genetic services.
For example, to make the patient experience of care more streamline, one health system in Des Moines, Iowa, has adopted an innovative genetic services model that combines cancer risk assessment and management software with telehealth genetic counseling services. "Rather than refer these patients elsewhere for genetic counseling - which studies show can be a significant barrier to care - we wanted to bring personalized genetic counseling services to them and create a seamless patient experience," said the director of oncology services in a GenomeWeb report.
To improve the health of populations, one West Coast-based health system is bringing genetics into routine care settings like OB/GYN and primary care. The system integrated cancer risk assessment and management software into its Cerner EMR to streamline a multi-specialty rollout. In doing so, the health system is screening according to National Comprehensive Cancer Network (NCCN) guidelines. If a patient is high risk, they are offered enhanced cancer screening services (e.g., MRI) and, if appropriate, preventive surgeries. For patients at average risk, undergoing the genetic evaluation process makes cancer prevention more top of mind and helps improve mammography and colonoscopy screening rates.
To truly understand how genetics reduces the average cost of care per patient, one San Diego-based health system focuses on three areas:
- Downstream revenue from increased surveillance and preventive services
- Staff efficiency to increase operating capacity and reduce average cost per a patient consult
- Averted or reduced costs from future/subsequent cancers
Learn More
Interested in learning more about how cancer risk assessment, genetics, and innovation help providers achieve the Triple Aim? Download the full white paper.
