Preventing primary and secondary cancer diagnoses through better screening
High-risk breast centers can now offer a personalized and precise approach to breast cancer prevention and treatment, detecting patients at high risk of hereditary breast cancers early, or even before the cancer has a chance to develop.
But patients at higher risk of developing breast cancer may be genetically prone to other cancers as well — and the screening associated with the high-risk breast center can identify those anomalies, too.
Prioritizing patients for genetic testing
Millions of women with a family history of breast or ovarian cancer have yet to undergo genetic testing, even though their lifetime risk of disease could be seven times higher than average if they have certain genetic mutations.
Health systems with a high-risk breast program can identify patients who are eligible for genetic testing based on family history and other factors. For instance, CancerIQ’s software uses the NCCN guidelines for genetic/familial high-risk assessment to find eligible patients and seamlessly flag them for their care team.
If a patient is eligible, she can undergo a full panel test, which is now standard of care instead of a single gene test. A full panel test looks for mutations in several genes, grouped into categories based on medical concern. Such a test could look for mutations in BRCA1 and BRCA2 genes — known to put women at high risk of developing breast cancer — and also for mutations in other genes. For instance, the PALB2, PTEN, TP53 genes are being studied for their association with hereditary breast cancer, too.
Impact beyond breast cancer
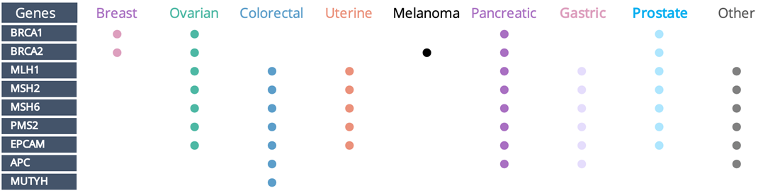
A full panel genetic test can find mutations associated with breast cancer, but it can also uncover mutations that could put the patient at risk for other types of hereditary cancer.
BRCA1 and BRCA2 mutations, for example, are also associated with ovarian, pancreatic and prostate cancers, in addition to putting a patient at high risk for breast cancer.
A full panel test may find no BRCA mutations but could find mutations in genes like MLH1 or MLH2, which are associated with ovarian, uterine, colorectal cancer and more.
This knowledge can empower patients and their care teams to discuss the findings together and create appropriately customized screening and preventative care plans.
So when a health system implements a high-risk breast program, that program has ripple effects into other cancer types. One such health system is CHRISTUS Ochsner in Louisiana, which built a high-risk breast program with the ripple effect top of mind.
“Patients at high risk of breast cancer are commonly at risk for other types of cancer, too. At Ochsner, we wanted to build a safety net for those patients, so we designed a high-risk breast program with CancerIQ,” said Dr. Alice Prestia, an OB-GYN with CHRISTUS Ochsner Lake Area Hospital.
CancerIQ’s new ebook, The Definitive Guide to High-Risk Breast Programs: How a Modern Approach to Design and Implementation Drives Better Clinical and Financial Outcomes, can help cancer prevention professionals start or grow their own high-risk breast program and ensure patients aren’t left asking “why didn’t someone detect this sooner?”.
Download the brand new ebook for free here.