Three months ago, health systems were embracing precision health strategies, and capturing the full clinical and financial value of using genetics in routine care. That’s before COVID-19 forced every US health group to close their doors to most patients. Not only is the health of every US citizen now in question, but also the financial health of every medical practice.
Ensuring the financial security of your system requires an important, but not too radical shift in priorities. A prioritization in proactive measures while we're all learning hard lessons and consequences of reactive measures.
This is a warning against shutting down the precision prevention services that have helped improve outcomes of high risk patient populations. Cancer screening services and genetic testing have led to early diagnoses and fewer cancers - and we shouldn't take that for granted.
One of the big concerns that comes to mind is if we’ll see more late-stage diagnoses across the next year or two, resulting in poorer outcomes. Cancer screenings have come to a halt and I for one can't predict when they'll start back up again.
- Dierdre Saulet, Expert Partner at Advisory Board
In this blog we’ll show you why it’s vital to keep your genetics program active, and even elevate its importance within your organization, to stay above water. Continue investing in your organization before it’s too late. And after a March where Colon Cancer awareness month saw its star overshadowed by Coronavirus, let’s apply some of these principles to colon cancer.
Three important statistics regarding colon cancer that are worth highlighting.
Let’s connect a few dots. If Lynch syndrome is the leading risk factor for colon cancer, and it progresses far more quickly than traditional colon cancer, what does that have to do with COVID-19?
Cancer itself can weaken the immune system by spreading to bone marrow – where white blood cells are made. Cancer treatments can also weaken the immune system, and unfortunately those treatments are not rare. For instance, chemotherapy is the common standard treatment for any progressed disease. Targeted therapies and even steroid usage can impact the immune system.
Shutting down screening programs is not one gamble (possibly increasing late stage cancer diagnoses) it is a double jeopardy.
When the doors open back up, it is critical that practices have quantifiable means to prioritize high-risk patients. They’re simultaneously the ones who stand to bring in meaningful revenue as they are to drain a system with in-patient costs if not managed early and urgently.
The good news is that most systems have reacted in a way that’s left massive opportunity for this problem to be appropriately addressed. In some systems there are up to 50% of staff - not working the front lines to treat COVID-19 symptoms - that are on payroll but planted at home sitting idle.
Patients are stuck at home too, concerned for their overall health; more on that later. For now, here’s how we propose you get started.
Maintain engagement with high risk patients that may fall through the cracks
We’ve observed that high risk patients without a personal cancer history are already less likely to follow up with genetic counseling recommendations. In fact, fewer than one in five individuals with a family history of breast cancer or ovarian cancer have undergone genetic testing.
The most effective way to engage these patients is within 2 weeks of a referral, as no show rates dramatically increase thereafter[1]. Between now and next year’s visit – a hereditary cancer could not only emerge, but grow pretty fast[2].
Engaging patients remotely while health is top of mind is not only the best way to stay ahead of COVID-19, but also ahead of cancer. And since those who are immunocompromised are at a greater risk to COVID-19, your work identifying and treating cancer early is also helping population health efforts given the uncertainty of where COVID-19 cases will be at 3-6 months from now.
[1] Rahm AK, Sukhanova A, Ellis J, Mouchawar J. Increasing utilization of cancer genetic counseling services using a patient navigator model. Journal of genetic counseling. Apr 2007;16 (2):171-177.
[2] Guindalini R., et al. Intensive surveillance with bi-annual dynamic contrast-enhanced magnetic resonance imaging downstages breast cancer in BRCA1 mutation carriers. Clinical Cancer Research. 2019 Mar 15; 25 (6): 1786–1794.
Use Your Available, Idle Resources
This is a good time for genetic counselors, physician assistants, or any adequately trained professional to mitigate or get on top of the backlog that’s already accumulating. Preventing a backlog is going to be key to your program surviving after COVID-19. Those patients already reticent about coming in won’t have the patience to join a 6 week waiting list, they will seek care elsewhere – a direct to consumer group or the nearby system who’s already taking this advice.
There’s also the virtual route, which we and other companies can assist with.
The Financial Justification
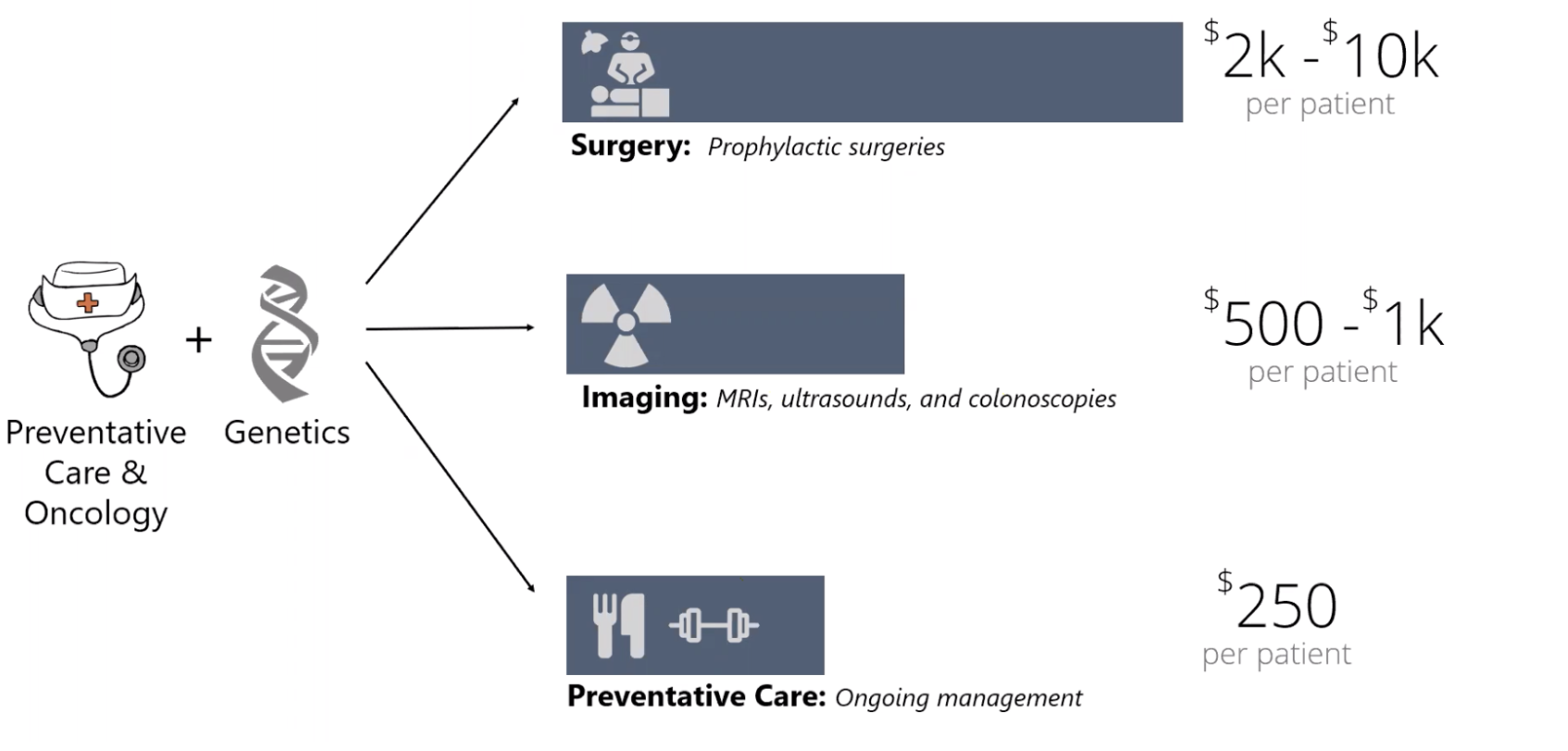 In a fee-for-service model, halting elective services comes as a huge financial hit. A telehealth genetics program can continue screening patients and delivering care remotely, and build a pipeline of patients for preventative surgeries and screenings when services return.
In a fee-for-service model, halting elective services comes as a huge financial hit. A telehealth genetics program can continue screening patients and delivering care remotely, and build a pipeline of patients for preventative surgeries and screenings when services return.
If you are in a fee-for-value model, later stage diagnoses and delayed treatment lead to escalating overall costs. Continuing to engage with patients and navigate the patients already classified at risk is also aligned with your values and business model.
Positive Trends
There are a few positive trends right now that we believe will make some people more open to setting an appointment. These factors include:
- Patients are thinking about their health more than ever - In the same way people are paying more attention to social distancing, washing their hands, and wiping down surfaces, they are more interested in monitoring other health risks. Filling out a hereditary cancer risk questionnaire may have been off the radar a month ago, but now they're more open to the process.
- Patients are speaking with their family - There is more time right now to reach out to parents, grandparents, uncles/aunts to gain a more accurate picture of the family medical history. This can be one of the topics that comes up in conversation when a patient is filling out their family history.
- You don't have to convince your patients to come in - No driving. No parking. No wait time. You may find people are more open to a virtual appointment than in-person.
CancerIQ’s Commitment To You
At CancerIQ, we want to help you transition to virtual appointments during this challenging time because we believe these transitions will also help you in the future as patients become more comfortable and even start to demand telehealth services.
To help in all this, we are offering the CancerIQ Specialist for 90 days for programs seeking an immediate solution to continue to care for patients during this time. We know caring for your patients who are at high-risk or who have cancer can’t wait, but as many patients as possible need to stay home and stay safe. We are here to help providers overcome challenges, not to pose a new one.
If you are an existing CancerIQ client and want to learn more, contact Haibo Lu, VP of Product and Customer Success.
If you are a provider and would like to access the CancerIQ Specialist at no charge for the next 90 days, contact Kelly Hall, VP of Commercial Strategy.