Hereditary cancer risk assessment programs present an enormous value proposition for health systems. In the short-term, it can drive additional revenue through increased surveillance and preventative services. Over the long term, health systems can catch cancers earlier - or prevent them altogether - reducing the overall cost of care.
As well, accreditation bodies like the National Accreditation Program for Breast Centers (NAPBC) or the Commission on Cancer (COC) require risk assessment, genetic counseling, and genetic testing.
In a fee-for-service and fee-for-value environment this is a win-win. Despite the clear incentives, however, health systems nationwide struggle to implement and scale effective cancer risk assessment programs. Specifically, there are four major challenges:
- Identifying eligible patients
- Navigating patients to genetic services
- Seeing patients in a timely manner
- Managing patients classified at risk
This was the focus of the recent webinar, Scaling Genetic Cancer Risk Assessment Across the Health System. Throughout, we discussed real-world insights and best practices for maximizing the value of offering comprehensive genetic counseling and testing services. Here are the key takeaways:
How to Identify More High-Risk Patients
Flagging patients who are eligible for genetic evaluation is typically a manual process that is error-prone and time consuming. Common practices include collecting family history on paper intake forms, using the radiology information system or EMR, or verbally asking patients about their family history. But these methods have proven ineffective, and a more patient-centered approach is needed.
One solution is to adopt a digital risk assessment tool. That's what Riverside Healthcare breast center in Kankakee, Illinois, did, reported Health Data Management.
In September 2017, Riverside Healthcare breast center switched from a paper process to software for identifying patients who are at increased or high risk for hereditary cancers. In doing so, the center simplified the screening process, could immediately determine which patients were at risk, and reduced the stress levels for both patients and mammography technicians. Additionally, they more than doubled the number of patients identified as eligible for MRI surveillance.
Want to learn more about how a digital risk assessment tool can benefit you? Watch the 8-minute video:
How to Navigate Patients to Genetic Services
The primary reason health systems implement a screening process is to identify patients who are eligible for genetic counseling and testing. It's about getting those patients from point A (e.g., imaging centers, oncology, gastroenterology, OB/GYN, primary care providers) to point B, the genetic specialist. However, within that process, patients begin to drop off.
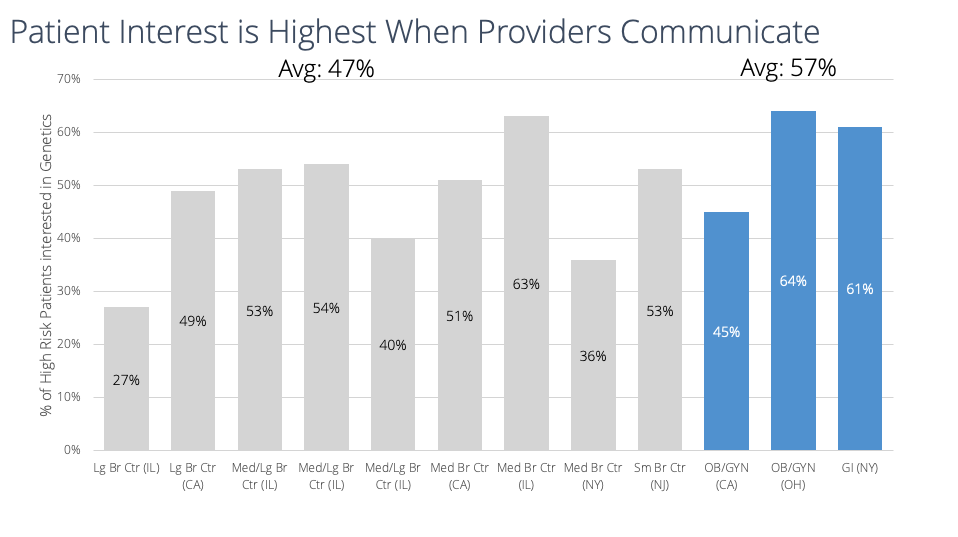
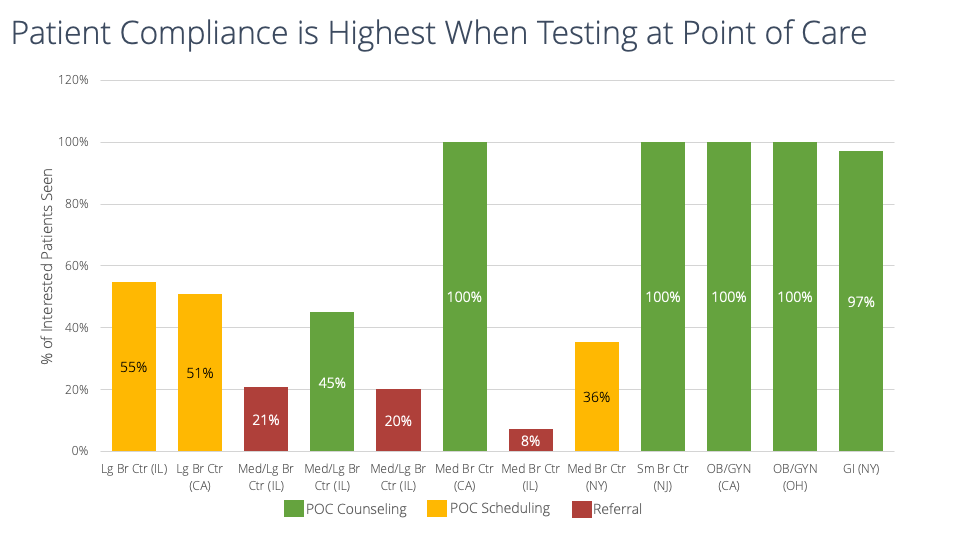
From the work we've done at health systems across the country, there are two main drivers that (a) impact the patient's interest in genetics and (b) improve the patient's compliance with genetic counseling and testing.
To increase patient interest in genetic services, it matters who communicates. Based on data from 12 different sites, we found that patient interest is highest when providers communicate to them about genetics, compared to non-provider staff.
From those same 12 sites, we also found that patient compliance for genetic services is highest when testing is completed at the point of care. This is compared to other models of implementing genetic services like referring out to a genetic counselor.
For a deeper dive into better navigating patients and increasing uptake for genetic services, watch this 13-minute video:
How to Increase Your Genetics Service Capacity
We know how to prevent hereditary cancer, but the process is far too costly and time consuming. In fact, the average initial genetic counseling appointment lasts nearly four hours, reports the National Society of Genetic Counselors (NSGC). An appointment may consist of gathering a patient's family history, drawing a pedigree from scratch, ordering diagnostics, writing letters for insurance pre-authorization, and generating patient notes.
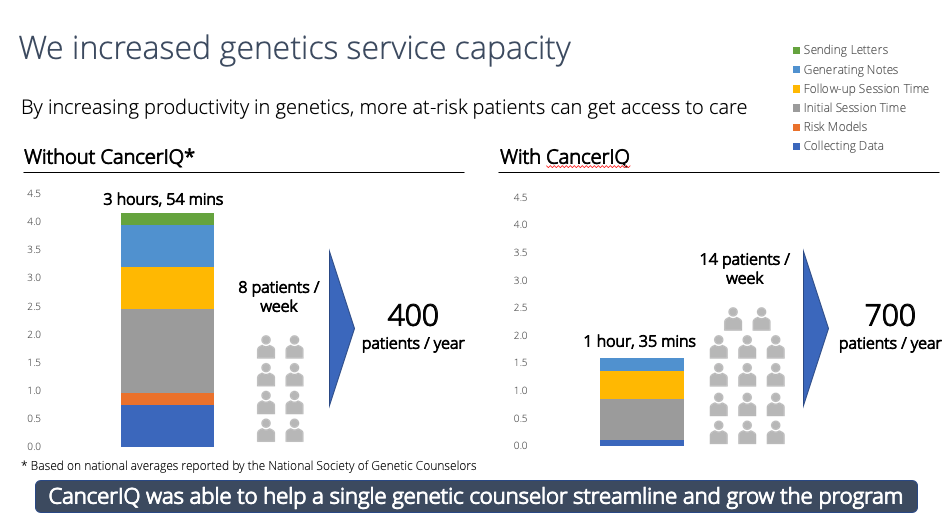
While some health systems might hire additional staff to increase their genetics service capacity, others are turning to innovative solutions to streamline and standardize their genetic counseling process.
Take Sharp HealthCare, for example. According to an Advisory Board report, after implementing specialty software, Sharp increased access to their genetic counseling services by 40 percent, going from 633 patients consulted in 2017 to 895 consulted in 2018. And they achieved this without additional hires and without burning out current staff.
How can you maximize your genetic specialist resources without burning them out? Watch the 10-minute video to learn more:
Managing Your High-Risk Patients Over Time
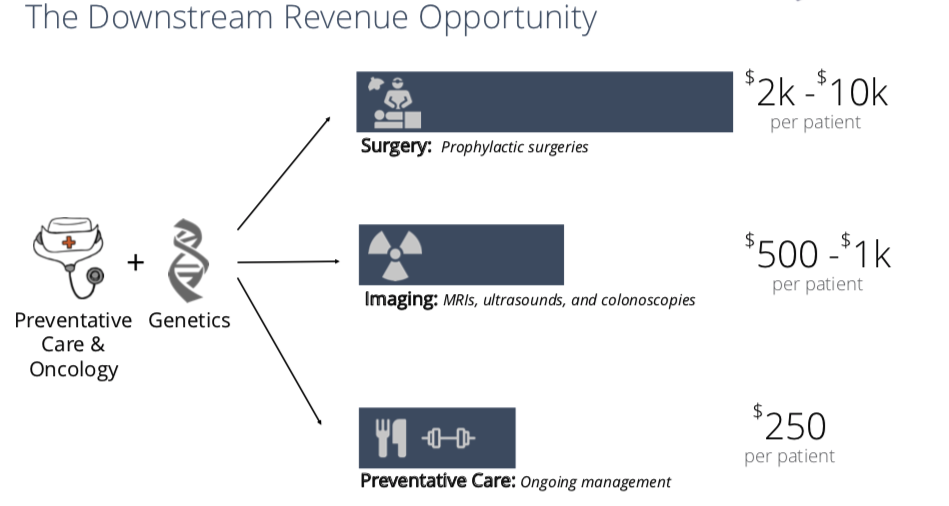
There is an enormous downstream revenue opportunity that comes from a population genetics risk assessment strategy. Once you flag high-risk patients and navigate them to genetic services, your system can generate incremental revenue on the resulting preventive care - more so than what a health system would make on genetic counseling appointments alone.
Watch the 6-minute video to learn how to quantify the impact on downstream revenue from genetic services:
Next Steps: Getting Buy-In From Leadership
Expanding cancer risk assessment, genetic counseling, and genetic testing services across your health system must be implemented thoughtfully.
- Start your program in places where cancer screening is already top of mind (e.g., breast imaging or gastroenterology), and grow into sites where professional society guidelines support genetic testing (e.g., oncology or OB/GYN). From there, you can continue to bring more providers on board from primary care settings.
- Establish a multi-specialty group of physicians to help improve care coordination and drive better outcomes for high-risk patients. That's exactly what West Coast-based Adventist Health has done, reported Fierce Healthcare. Patients who are identified as high risk are navigated to regional "circles of care," which are formed by Adventist Health specialty groups - including gynecology, urology, oncology/hematology, dermatology, breast surgery, gastroenterology, and psychology.
- Forecast the downstream revenue opportunity using hard metrics to gain buy-in from the financial decision makers within your organization. Pair your return on investment (ROI) analysis with real case studies of success from other health systems, and you will be on your way to building greater confidence with senior leadership.
How can you get stronger buy-in to scale your cancer risk assessment program? Watch the 6-minute video to learn more:
Learn More
Interested in learning more? Watch the full webinar Scaling Genetic Cancer Risk Assessment Across the Health System.



